Repair or Replacement of Defective Direct Composite Restorations: A Survey of Dentists
OBJECTIVE: The criteria for repair of composite restorations are controversial. This study investigates the knowledge and the current practices of dental graduates about the repair of resin-based composites.
METHODOLOGY: A questionnaire based survey was developed, seeking information about management (repair or replacement) of defective composite restorations and distributed among 200 dental graduates of four teaching dental hospitals in Lahore.
RESULT: The decision to choose composite repair as a treatment option in clinical practice was influenced by whether it was taught at undergraduate level. Sixty one percent of graduates reported that they were not taught composite repair at dental undergraduate level, as a result only 18% of these respondents chose repair in their clinical practice as a treatment option. The preferred indication for composite repair was secondary caries (37%) (p=0.010) followed by partial loss of composite restoration (29.5%), fracture of composite (21%) and composite discoloration (12.5%). Large number of respondents (73%) agreed that repair increased longevity of a defective composite restoration. The results highlighted that knowledge and application of composite repair is significantly higher in experienced clinicians (p=0.003). Half of the participants considered that repair was less time consuming and 73% responder agreed that repair increased longevity of a previously restored defective composite restoration.
CONCLUSION: This study demonstrated that knowledge about composite repair rather than replacement requires serious consideration at undergraduate level as majority of dental graduates are not familiar with the concept and implication of composite repair. Didactic and clinical training component regarding composite repair should be added in dental curriculum to inculcate the knowledge of repair of composite restorations.
HOW TO CITE: Fayyaz A, Fareed MA, Ehsan S, Baig QA, Noor NA. Repair or Replacement of Defective Direct Composite Restorations: A Survey of Dentists. J Pak Dent Assoc 2015; 24(1):17-21.
INTRODUCTION
The recent advances in bonded restorative materials has persuaded minimally invasive treatment strategies for tooth preservation, reinforcement of the remaining tooth structure, better marginal seal and eventual increased life span of restorations1. In recent years, the extensive usage of resin-based composite restorative materials (RBCs) in clinical dentistry is attributed to its excellent aesthetics. The advent of RBCs with better mechanical properties and less shrinkage has led to their use in posterior teeth compared to amalgam2. Composite restorations have a number of advantages for example: conservation of remaining tooth, adhesion to tooth structure, strengthening of restored tooth unit, satisfactory aesthetics and ease of repair1. Directly bonded restorations commonly undergo marginal deterioration and are generally more susceptible to secondary caries. Consequently, a localized defect in a composite restoration is a common situation for dentists to decide between repair and replacement.Restoration repair is the partial replacement of a
defective restoration showing no clinical or radiographic signs of failure whereas restoration replacement is the complete removal of previous restoration followed by placing a new restoration1. Conventionally, a defective composite restoration was replaced but recently, repair is a conservative treatment option that has been advocated3,4. Complete replacement of a composite restoration may be considered unduly interventional in conditions where the restorations (>80%) may be found to be healthy clinically and radiographically5,6. The invariable outcome of restoration replacement and the unwarranted removal of sound tooth structure from sites that are unaffected by any localized defect result in the weakening of the remaining tooth structure. This along with the added possibility of pulpal insult results in acceleration of the “restoration death spiral”7. Moreover, patient factors also play an important role in the progression of defective restorations over an extended period of time8. This provides the clinician a chance to deal with the cause of the defect and to repair the restoration with minimal intervention thereby prolonging the lifespan of the restoration9.
There is substantial evidence validating the significance of procedures to repair defective restorations10. Since the last decade, an increase in placement of composite restoration in general dental practice resulted in increased evidence that repair rather than replacement is considered as a treatment option for defective composite restorations11. Therefore, aim of this study was to examine the extent of contemporary knowledge and practices about the indications of composite restoration repair among dentists working in various teaching dental hospitals in Lahore, Pakistan.
METHODOLOGY
A survey questionnaire (consisting 16 questions) was designed and distributed to 200 dental graduates in 4 teaching dental hospitals in Lahore Pakistan. Participants were informed that their demographics will be kept confidential. All designed questions seeking the information about composite repair were close ended. The survey items were pre-tested for ambiguity, content validity, reliability and clarity by the authors in their institute. The survey inquired about the knowledge, attitude and practices of treating a defective composite restoration. The survey also inquired for information about the most common indications of repair of a defective composite restoration. The returned questionnaires were coded and data wad entered and analyzed using Statistical Package for the Social Sciences (SPSS) Version 20.0. Descriptive and analytical statistics were used to analyze each variable and associations were tested for statistical significance using Chi-square tests at 95% significance level.
RESULTS
Completed questionnaire responses were received from four dental schools giving a response rate of 100% (200 participants). No incomplete responses were received. Eighty nine percent of the participants had less than 4 years of clinical experience [1-2 years = 107 (53.5%), 2-4 years = 70 (35%), 4-6 years = 20 (10%) and 6-8 years =3 (1.5%)]. Majority of dentists (64.5%) reported that they consider patients preferences for repair or replacement of the defective composite restoration. The most common indication for repair was secondary caries (37%) (p=0.010), followed by partial loss of composite
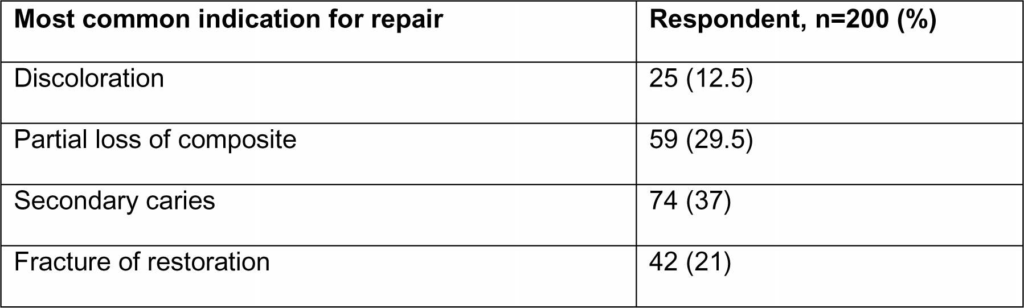 Table-1 Most common indications of composite repair in respondent’s clinical dental practice
Table-1 Most common indications of composite repair in respondent’s clinical dental practice
(29.5%), fracture of composite (21%) and 12.5% of the respondents selected composite discoloration as an indication for repair (Table 2). Sixty five percent chose
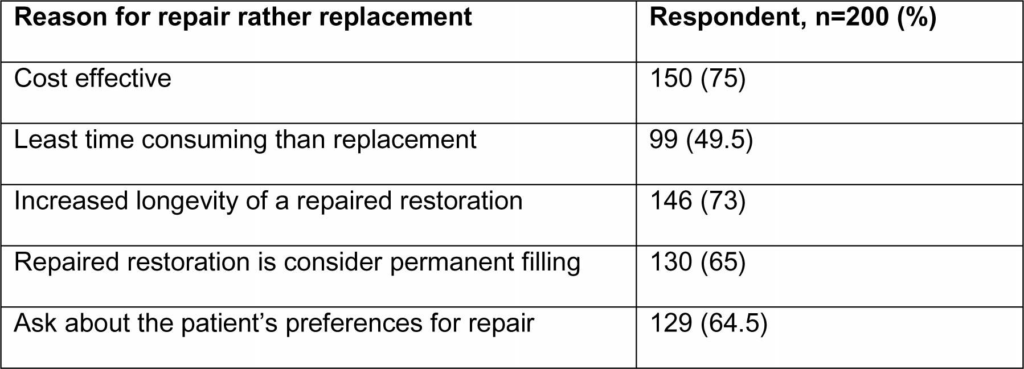 Table-2 Reason associated with the decision to repair defective composite restorations
Table-2 Reason associated with the decision to repair defective composite restorations
repair to treat a small defect in composite restoration. When enquired if repair was a less invasive treatment option as compared to replacing a composite restoration, 68% of the respondents agreed. Results of our study revealed that 49.5% of the participants thought repair was less time consuming than replacement of the whole composite filling. Table 3 shows that 73% responder
 Table-3 Participant’s treatment choice in a clinical scenario of a defective composite restoration.
Table-3 Participant’s treatment choice in a clinical scenario of a defective composite restoration.
thought that repair increased longevity of a previously done defective composite restoration. The large number of participants considered repaired restorations as permanent fillings (65%) whereas 30% considered repair as an intermediate filling and 5% considered it as a temporary filling. More than half of respondents 121 (60.5%) reported that they were not taught about composite repair during BDS training. However, 162 (82%) respondents have replaced a defective composite restoration and 121 (60.5%) have performed composite repair in their clinical practice as a treatment option (Table 4). The results
 Table 4. Response of participants to survey questions related to knowledge and practices of composite repair and replacement
Table 4. Response of participants to survey questions related to knowledge and practices of composite repair and replacement
showed that as experience of the dentist increased (3-8 years) the awareness of repair as a treatment option also increased (p=0.003) as well as repair being performed as a treatment (p=0.028).
DISCUSSION
As with all questionnaire-based surveys, risks exist in relation to the reliability of responses and the potential of non-response bias. Our study had a 100% response rate but the limitation of this study was the group (n=200) of dentists based in one city were questioned. Irrespective of this weakness the results are consistent with the findings of previously published studies4,6,12. Additionally, there is a strong agreement amongst academicians in conservative dentistry around the world that there are merits in repairing rather than replacing defective direct resin composite restorations7,8,12,13.
Hickel and Manhart argued that clinician factors, material properties and patient factors are responsible for repair or replacement of defective restoration14. The refurbishment is a minimal intervention approach to treat the defects which are superficial while localized defects which are accessible can be treated by repairing2,9. The benefit of this minimal interventional approach to treatment of defective restorations is a restored tooth with minimal removal of healthy tooth tissue which is stronger and better able to withstand functional loads resulting in better long term prognosis. A restoration that is replaced tends to be larger than the one it is replacing therefore, extensive restorations have shorter longevity than smaller restorations in clinical service10. Gordan et al. reviewed the data published regarding the repair of composite restorations and concluded that repaired restorations had higher survival rate; improved sealing of crevice or ditch with superior longevity when compared to restorations which remained untreated. These restorations showed marginal wear after 7 years11.
All restorative materials fail under masticatory loads of oral cavity and the annual failure rate of RBCs have been reported in lower range (2.2%)12-14. Therefore, Mjor reported that nearly half of the dental restorations were done to replace existing defective restorations15. The results of the present study suggest that the replacement of faulty restorations is regarded as a preferred alternative (82%). However, the longevity of a restoration is invariably affected by the choice of repair versus replacement of a defective composite filling16,17. Replacement of a previous large composite restoration is time consuming which may cause pulpal damage due to needless tooth structure destruction and also increases chances of tooth crown fracture12,18. Hence, some flawed composite restorations may be salvaged to increase longevity by repairing the composite restoration13. Performing restoration repair, if appropriate, may conserve tooth structure and is less time consuming due to better patient experience and in some cases needs no local anesthesia13. Defects in composite restorations which are sound both clinically and radiographically, are the most suitable candidates for performing repair; for example defects at the cavo-surface margin, secondary caries, partial loss and discolouration2,13. Kallio reported that repairing of old restorations leads to tooth tissue preservation and is more cost-effective than the removal and insertion of a new restoration19. This is in accordance with our finding in which 68% of the
respondents agreed that repair was less invasive than replacement. It is critical to select a minimally invasive treatment option for restorations that have already been done to increase the longevity of the tooth. The main reason for repair was found to be secondary caries (43%) by Gordon et al8 whereas the results of present study indicated that secondary caries (37%) was also the most common repair indication selected by the participants. Most universities in Europe (88%), USA (88%) and Scandinavia (92%) reported that they have included teaching of composite repair techniques in dental
curriculum13,12,20. Almost all universities regard repair as a minimally invasive treatment option resulting in delaying the degradation or failure of restorations22.
Tyas reported that repair was not the usual standard of care and considered it as “patchwork dentistry”23. Nonetheless, repair was considered a treatment of choice depending upon each case therefore, 50-71% dentists choose replacement rather than repair of the restorations. This is contradictory to our study in which 82% dentists performed replacement of composite restorations. However the findings of our study revealed that majority of dentists have not received didactic instructions about various factors during their undergraduate dental training to consider composite repair as a viable treatment option for defective restorations. Only 39% of dentists claimed that they were taught/trained the subject of composite repair during BDS and only 60% of participants recognized repair as a treatment option if required. When we inquired the dentists whether they have knowledge about composite repair, 61% replied positively as they have performed repair (60.5%) in their general dental practice.
CONCLUSIONS
There are many factors which may influence the choice to repair rather replace a defective composite restoration. Our study highlighted that the preferred choice as indication for composite repair was secondary caries and partial loss of composite restoration. More than two third of respondents agreed that repair increased longevity of a defective composite restoration. Based on the results of this survey, it is evident that most of the participants were not taught about the indications and techniques for repair of composite restorations as compared to other countries in the world. The results of this study also indicated teaching tooth restorative techniques influenced the practicing habits of dentists when considering treatment options of defective composite restoration.
RECOMMENDATIONS
It is suggested that teaching of composite repair should be vigorously implicated in teaching institutions of Pakistan as it is in the best interest of the patient. Dental students should be provided didactic and clinical training on this topic. Future research can be carried out for refining the guidelines and technique utilized for composite repair.
REFERENCES
- Blum IR, Jagger DC, Wilson NH. Defective dental restorations: to repair or not to repair? Part 1: direct composite restorations. Dent Update. 2011;38:78-84.
- Lynch CD, Wilson NH. Managing the phase-down of amalgam: part I. Br Dent J. 2013;215:109-113.
- Sharif MO, Catleugh M, Merry A, Tickle M, Dunne SM, Brunton P et al. Replacement versus repair of defective restorations in adults: resin composite. Cochrane Database Syst Rev. 2006;CD005970.
- Opdam NJM, Bronkhorst EM, Loomans BA, Huysmans MC.Longevity of repaired restorations: a practice based study.J Dent.2012;40:829-835.
- Gordan VV, Mjr IA, Blum IR, Wilson NHF. Teaching students the repair of resin based composite restorations: a survey of North American dental schools. J Am Dent Assoc. 2003;134:317-323.
- Gordan VV, Riley JL, Worley DC, Gilbert GH, The DPBRN Collaborative Group. Restorative material and other tooth-specific variables associated with the decision to repair or replace defective restorations: findings from the Dental PBRN. J Dent 2012;40:397-405.
- Blum IR, Lynch CD, Wilson NHF. Factors influencing repair of dental restorations with resin composite. CliniCosmInvesti Dent. 2014;6:81-87.
- Gordan VV, Riley JL, Geraldeli S, Rindal DB, Ovist V, Fellows JL. Repair or replacement of defective restorations by dentists in The Dental Practice-Based Research Network. JAm Dent Assoc. 2012:143:593-601.
- Gordan VV. Clinical evaluation of replacement of Class V resin based composite restorations. J Dent. 2001;29:485-488.
- Da Rosa Rodolpho PA, Cenci MS, Donassollo TA, Loguercio AD, Demarco FF. A clinical evaluation of posterior composite restorations: 17-year findings. Journal of Dentistry 2006;34:427-435. Fayyaz A / Fareed MA / Ehsan S / Repair or Replacement of Defective Direct Composite Baig QA / Noor NA JPDA Vol. 24 No. 01 Jan-Mar 2015 21
- Gordan VV, Garvan CW, Blaser PK, Mondragon E, Mjoer IA. A long-term evaluation of alternative treatments to replacement of resin-based composite restorations: results of a seven-year study. J Am Dent Assoc. 2009;140:1476-1484.
- Lynch CD, Frazier KB, McConnell RJ, Blum IR, Wilson NHF. Minimally invasive management of dental caries: contemporary teaching of posterior resin – based composite placement in U.S. and Canadian dental schools. J Am Dent Assoc. 2011;142:612-620.
- Blum IR, Lynch CD, Wilson NHF. Minimally invasive management of defective composite restorations: Contemporary teaching of composite restoration repair in Scandinavian dental schools. J Oral Rehab. 2012;39:210-216.
- Manhart J, Chen H, Hamm G, Hickel R. Review of the clinical survival of direct and indirect restorations in posterior teeth of the permanent dentition. Oper Dent 2004;29:481-508.
- Mjor IA, Moorhead JE, Dahl JE. Reasons for replacement of restorations in permanent teeth in general dental practice. Int Dent J. 2000;50:360-366.
- Goldstein GR. The longevity of direct and indirect posterior restorations is uncertain and may be affected
- by a number of dentist-, patient-, and material-related factors. J Evid Based Dent Prac. 2010;10:30-31.
- Hickel R, Manhart J. Longevity of restorations in posterior teeth and reasons for failure. J Adhes Dent.
- 2001;3:45-64.
- Yousef MK, Khoja NH. Repair and replacement perception of dental restorations. Med Sci J. 2009; 16:75-85.
- Kallio TT, Tezvergil-MutluayA, Lassila LVJ, Vallittu PK. The effect of surface roughness on repair bond strength of light-curing composite resin to polymer composite substrate. Open Dent J. 2013;7:126- 131.
- Blum IR, Lynch CD, Wilson NH. Teaching of direct composite restoration repair in undergraduate dental schools in the United Kingdom and Ireland. Eur J Dent Educ. 2012;16:53-58.
- Lynch CD, Blum IR, Frazier KB, Haisch LD, Wilson NH. Repair or replacement of defective direct resin-based composite restorations: contemporary teaching in U.S. and Canadian dental schools. J Am Dent Assoc. 2012;143:157-163.
- Hickel R,Brshaver K, Ilie N. Repair of Restorations-Criteria for Decision Making and Clinical Recommendations. Dent Mater. 2013;29:28-50.
- Tyas MJ, Anusavice KJ, Frencken JE, Mount GJ. Minimal intervention dentistry – a review, FDI Commission Project 1-97. Inter Dent J. 2000;50:1-12.

